Top 4 Ways Caregivers Can Prevent Bedsores


I’ve worked with caregivers for years and one of the greatest fears I hear expressed is of skin breakdown. The common belief is that bedsores are a sign of poor care or neglect. It feels like the badge of a bad caregiver. While that may be the case in some instances, more often than not, that couldn’t be further from the truth.
Now, this is not to downplay the seriousness of bedsores and the need to vigilant in prevention. They can be extremely painful and uncomfortable, challenging to heal once they start, and a portal for very serious infection. So, let’s explore the cause of bedsores and the top tips to prevent them.
What causes bedsores and how can they be prevented?
Bedsores, also known as pressure ulcers or decubitus ulcers are most commonly caused by prolonged pressure. Those most at risk are people who spend a significant amount of time sitting or lying.

Disclosure: Please keep in mind that some of the links in this post are affiliate links and if you go through them to make a
purchase I will earn a commission. I link to these companies and their products because of their quality and not because of the commission I receive from your purchases at no additional cost to you. The decision is yours.
Medical Disclaimer: The information on this site is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH THIS WEB SITE.
How can you prevent bedsores
1. Change Positions Frequently
The name pressure ulcer is not a coincidence. They are ulcerations, caused by pressure. So, naturally, the best way to prevent pressure ulcers is by relieving pressure. The easiest way to do this is by changing positions frequently. The image above shows some of the most common pressure points. By changing positions frequently and redistributing one’s weight, the high-risk pressure areas have time to revascularize and get blood flow to those compromised areas.
Ambulatory-For someone who has that ability to ambulate, it is simple as getting them up for short walks and bursts of exercise. Make sure they aren’t spending too much time in bed, the couch, or their recliner. If they have difficulty with mobility while in bed, help them turn every 2 hours. This also goes for the time spent napping in the recliner or watching television.
Wheelchair-Bound For those who are wheelchair-bound, encourage lying down after meals or in the afternoons. Maybe try alternating from the wheelchair to the recliner or bed, where you can reposition them more easily and relieve pressure.
Bedbound– For those who are bedbound, you have to be especially vigilant. As you can see from the photo above, there are multiple points of pressure that are constantly being compressed while in bed, if you don’t make a conscious effort to frequently reposition. The gold standard is turning and repositioning every 2 hours.
2. Keep Skin Clean and Moisturized
Good hygiene is of utmost importance. Not only will it help prevent the deterioration of skin cells, but it will also decrease the risk of infections, such as urinary tract infections and skin infections.
- Bathing Be sure to keep up with a regular bath or shower routine, washing every crevice and fold with mild soap and warm water. After bathing, make sure all of these areas are properly dried.
- Skin Assessment After bathing, this is the perfect time to assess the skin for any rashes, reddened areas, dry scaly areas, or any breaks in the skin. If you find any areas of concern, note them down. Even consider taking pictures, for the purposes of comparing, if things worsen or improve. While this may be helpful for you, it may also be helpful to a provider, when he or she is trying to get an accurate history and timeline, if skin breakdown does occur.
- Moisturize– After the skin has been cleaned and assessed, apply a good moisturizer. Dry skin can lead to small cracks and fissures in the skin, which can be portals for bacteria and infection. I often add moisturizes such as Eucerin or Aquaphor to my nursing home patient’s daily treatment orders, or otherwise, this simple preventative step can get missed.
- Incontinence Care When caring for someone with incontinence, it is extremely important to keep them clean and dry. Find a good adult brief that works for both of you. Using adult wipes are perfect for a quick clean up and extremely convenient, leaving very little to clean up, a warm soapy washcloth works just as good. Be sure to wash those towels on the hot cycle and consider using bleach. Check out my full post on incontinence care here.

- Barrier Creams and Ointments When caring for someone who is frequently incontinent, consider using an ointment such as, A&D ointment, just as a preventative barrier, to protect the skin against moisture. If the skin is showing signs of redness or irritation, consult their physician for recommendations. They may recommend creams such as Calmoseptine, Desitin, or other OTC products. If the skin is broken, draining, hot or inflamed, or if you notice a foul order or presence of a fever, notify the PCP immediately.
3. Offload
Offloading goes hand in hand with changing positions frequently. To offload is to relieve pressure.
1 Pillows– The simplest ways to offload are to use pillows to relieve pressure to high-risk areas. For example, propping pillows underneath the legs, leaving the feet slightly suspended in the air, thus relieving the pressure on the heels of the feet. Another common use of pillows is to roll the person to one side, propping the pillows under their back, to relieve pressure on the buttock and one hip at a time. This same concept can be applied to multiple areas of the body. So, stock up on pillows and waterproof pillow protectors, like ones below.
2. Chair cushions– For those who spend the bulk of their day sitting in a chair, finding a good chair cushion is critical. I would recommended asking their PCP for a prescription for a chair cushion and taking it to a medical equipment supplier. Be mindful that some suppliers may not be in their network. This can be a hassle and time-consuming. Here are a few of my top recommendations you can find on Amazon from $10-$65.
3, Mattresses and overlays Just like those chairbound, if you are caring for someone who spends more than 8 hours per day in bed or has limited mobility while in bed, you’ll want to find a mattress or mattress overlay that reduces pressure. This is another item that may or may not be covered by insurance. Again, ask their PCP if this is appropriate and then you can get the proper prescription for purchase or rental. Your loved one may also qualify for a hospital bed, which can helpful with frequent repositioning. If you choose not to go through medicare or private insurance or don’t qualify, consider an alternating pressure pad like this one below.
4. Good Nutrition
This preventative measure is often overlooked but can be one of the most vital preventative steps. Most don’t think of it as such, but the skin is an organ, in fact, it is the body’s largest organ. Organs need good nutrition to thrive.
1 Protein– Protein is critical for cellular growth and regeneration. Good sources of protein include meats, such as beef, pork, poultry, fish and eggs. Greek yogurt and cheese are also good sources of protein and can easily be incorporated into other meals. Non-animal sources of protein include nuts and nut butters, tofu, quinoa, lentils, chia seeds, and beans. You can make use of protein shakes, adding in additional fruits, greens, seeds, peanut butter or even ice cream to enhance the flavor.
2. Vitamins and Mineral -The best sources of vitamins and minerals are going to be from fresh fruits, vegetables, lean meats, whole grains, and dairy. Unfortunately, it’s not always feasible to get an aging adult to take in all of these nutrients. Again, get creative with shakes and smoothies and consider adding a high-quality multivitamin with added minerals.
3. Water – External moisturizers are one thing, but true hydration comes from the inside. Try encouraging 500 ml of liquids with meals and a minimum of 250 ml between meals, unless instructed otherwise by a provider. While water is best, decaf teas, coffee, juice, and soft drinks are okay as well. Try to avoid too much caffeine, as it can act as a diuretic and bladder irritant, causing dehydration over time.
How do you treat bed sores at home?
If despite your best efforts, a pressure ulcer still develops, consult a provider as soon as possible. The doctor may want to assess the wound for himself/herself or set up homecare to treat and monitor the wound. Until a professional can assess the area, I recommend cleaning the wound with normal saline or wound cleanser, patting dry with clean gauze, and then applying a clean dressing of gauze and non-irritating tape. Change the dressing daily or more often if the dressing is saturated or soiled. Do not apply any topical medication to the wound, unless instructed to do so by a medical professional. You could cause further damage to the tissue. Again, consider taking photos, and documenting the appearance of the wound’s location, size, color, drainage, and smell.
I know what you are thinking, “where would I get all of these items from?” All of these items can be found at your local drugstore, Target, or Walmart. However, I’m sure you’ve already experienced as a caregiver, things happen at the most inopportune times. So, I recommend having a wound care emergency kit prepared. You’ll need:
- Gauze

- Normal Saline or Wound Cleanser

- Abd pads

- Hypoallergenic Cloth tape

What pressure ulcers look like?
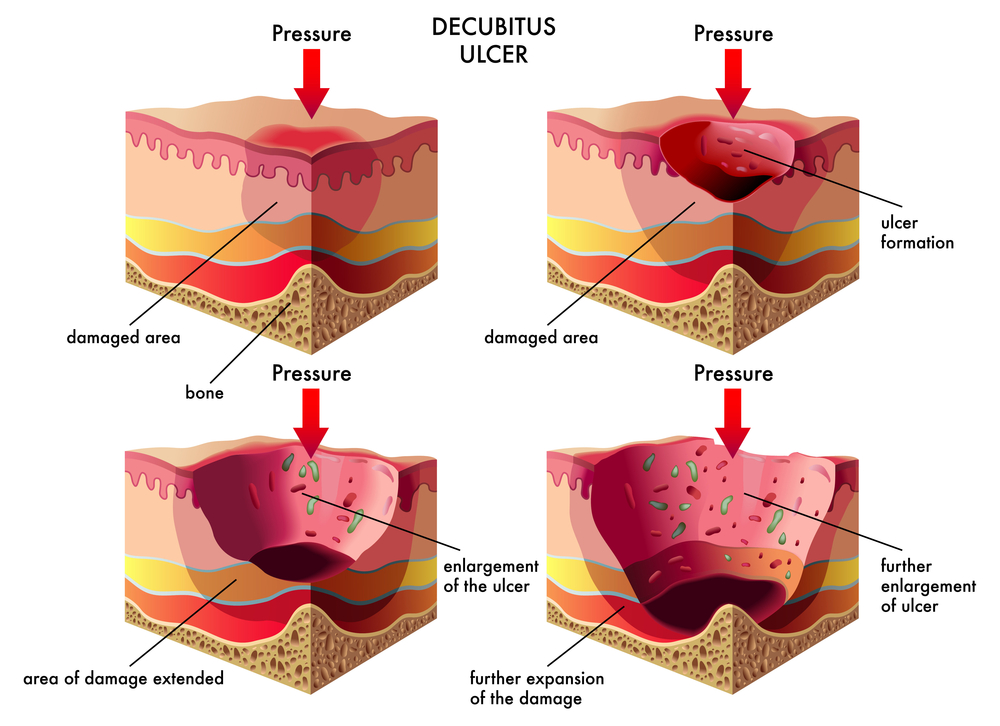
4 Stages of Pressure Ulcers
Stage 1 There is no break in the skin. However, the skin is reddened or discolored in a darker-skinned person, and oftentimes painful. They do not blanch when pressed. The area may be softer or firmer than the surrounding areas. These are the first signs of a pressure ulcer.
Stage 2 This stage involves a break in the top layer of skin or ulcerations. These wounds are typically shallow, but can be very painful.
Stage 3 In this stage the damage goes down to deeper levels of the tissue and may even expose fat tissue.
Stage 4 This stage involves deep, extensive tissue damage down to the tendons, muscles, and even bones.
Unstageable The wound can also be considered unstageable. This is when there has been a deep tissue injury (DTI), that is impossible to know the full extent of without imaging, or when there is dead tissue left behind covering the wound, thus also making it impossible to see the full extent.
In Summary
To recap, the best way to prevent pressure ulcers is to change positions frequently, offload or shift the pressure, keep the skin dry and moisturized, and concentrate on good nutrition. However, sometimes despite your best efforts, the skin breaks down anyway. Just like any other organ, sometimes it just fails. Don’t beat yourself up. Keep the area clean and dry and seek medical attention ASAP.
I hope this guide helps. Let me know your thoughts in the comments below and don’t forget to pin this post. For more content like this subscribe below.
As always, Be Blessed!
Stephanie